
Patients who receive a gynaecological cancer diagnosis experience significant consequences that extend beyond their physical health, affecting their emotional state and overall quality of life. Confronting the challenge of delivering comprehensive support to these women is essential, promoting a conducive environment for the disease process and enhancing their experience throughout the course of treatment and recovery.
Comprehensive support, as defined by the Hub, encompasses an understanding of six primary areas that significantly influence a patient’s life within the care process: physical activity, nutrition, sexuality, fertility, mental health, and employment. To deliver comprehensive support, it is imperative to recognise the distinct characteristics of every patient, which calls for a customised approach that addresses their specific requirements.
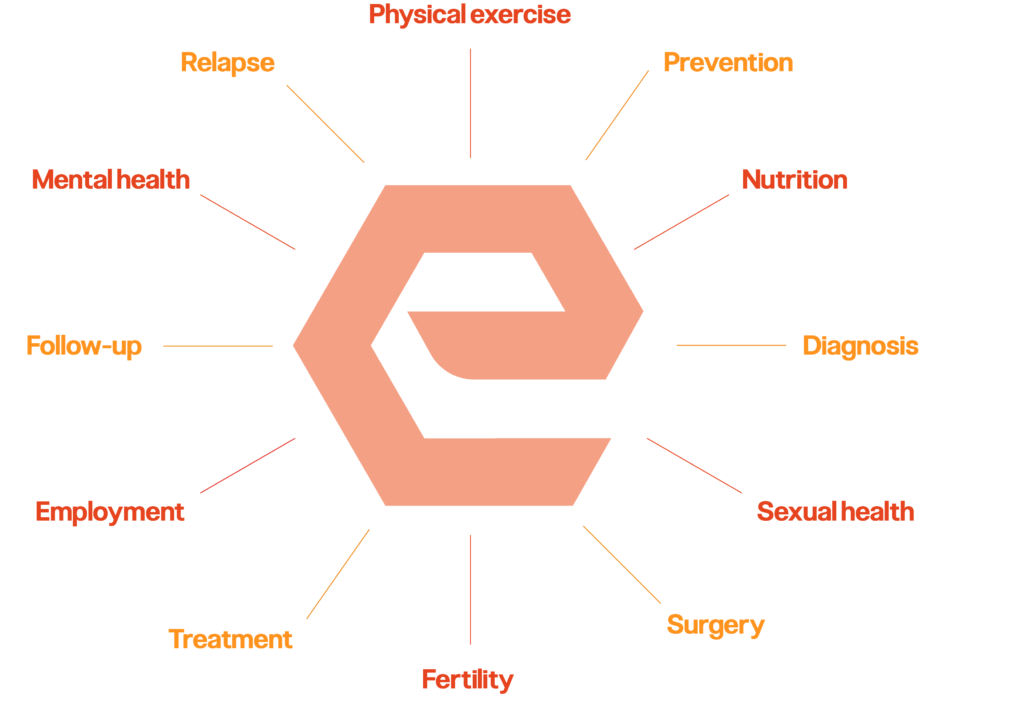
An in-depth examination of each aspect comprising this hexagon is justified:


It is imperative to underscore that support does not conclude with the completion of treatment. A comprehensive approach mandates continuous care throughout the patient’s life cycle, adapting to evolving needs during recovery or potential relapses.
The Hub endeavours to contribute to this area by facilitating access to validated, reliable information in a centralised manner. Collaboration with healthcare professionals from diverse disciplines, including oncologists, psychologists, social workers, nutritionists, coaches, therapists, and any other stakeholders driven by the challenge, is sought to generate ideas or solutions aimed at enhancing patient support.
Referencias:
[1] Zorlini, R., Akemi Abe Cairo, A., & Salete Costa Gurgel, M. (2008). Nutritional status of patients with gynecologic and breast cancer. Nutrición Hospitalaria, 23(6), 577-583. https://scielo.isciii.es/scielo.php?pid=S021216112008000800009&script=sci_abstract&tlng=pt
NP-ES-AOU-WCNT-240004 (v1) 02/2024

For more information, please contact your healthcare professional.
NP-ES-AOU-WCNT-240001 (v1) 02/2024